Prenatal development

Definition
Prenatal development refers to the process in which a baby develops from a single cell after conception into an embryo and later a fetus.
Description
The average length of time for prenatal development to complete is 38 weeks from the date of conception. During this time, a single-celled zygote develops in a series of stages into a full-term baby. The three primary stages of prenatal development are the germinal stage, the embryonic stage, and the fetal stage.
Germinal stage
Conception occurs when the female egg (ovum) is fertilized by a the male sperm. Under normal circumstances, one egg is released approximately once a month from a woman's ovary during a process called ovulation. The egg makes its way into a fallopian tube, a structure that guides the egg away from the ovary toward the uterus. For fertilization to occur, sperm ejaculated during sexual intercourse (or introduced during artificial insemination) in a substance called semen must have made their way from the vagina into the uterus and subsequently into the fallopian tube where the ovum has been released. This process can take up to ten hours after ejaculation. For fertilization to occur, a sperm must penetrate the tough outer membrane of the egg called the zona pellucida. When one sperm successfully binds with the zona pellucida, a series of chemical reactions occurs to allow only that sperm to penetrate. Fertilization occurs when the sperm successfully enters the ovum's membrane. The genetic material of the sperm and egg then combine to form a single cell called a zygote and the germinal stage of prenatal development commences.
The zygote soon begins to divide rapidly in a process called cleavage, first into two identical cells called blastomeres, which further divide to four cells, then into eight, and so on. The group of diving cells begins to move along the fallopian tube toward the uterus. About sixty hours after fertilization, approximately sixteen cells have formed to what is called a morula, still enclosed by the zona pellucida; three days after fertilization, the morula enters the uterus. As cell division continues, a fluid-filled cavity called a blastocoele forms in the center of the group of cells, with the outer shell of cells called trophoblasts and an inner mass of cells called embryoblasts. The zona pellucida disappears and the morula becomes a blastocyst. At this stage the blastocyst consists of 200 to 300 cells and is ready for implantation.
Implantation, the process in which the blastocyst implants into the uterine wall, occurs approximately six days after conception. Hormones secreted from the mother's ovaries and a chemical secreted by the trophoblasts begin to prepare the uterine wall. The blastocyst first adheres to the wall then moves into the uterine tissue. Implantation marks the end of the germinal stage and the beginning of the embryonic stage.
Embryonic stage
The embryonic stage begins after implantation and lasts until eight weeks after conception. Soon after implantation, the cells continue to rapidly divide and clusters of cells begin to take on different functions (called differentiation). A process (gastrulation) leads to the formation of three distinct layers called germ layers: the ectoderm (outer layer), the mesoderm (middle layer), and the endoderm (inner layer). As the embryo develops, each germ layer differentiates into different tissues and structures. For example, the ectoderm eventually forms skin, nails, hair, brain, nervous tissue and cells, nose, sinuses, mouth, anus, tooth enamel, and other tissues. The mesoderm develops into muscles, bones, heart tissue, lungs, reproductive organs, lymphatic tissue, and other tissues. The endoderm forms the lining of lungs, bladder, digestive tract, tongue, tonsils, and other organs.
The process of differentiation takes place over a period of weeks with different structures forming simultaneously. Some of the major events that occur during the embryonic stage are as follows:
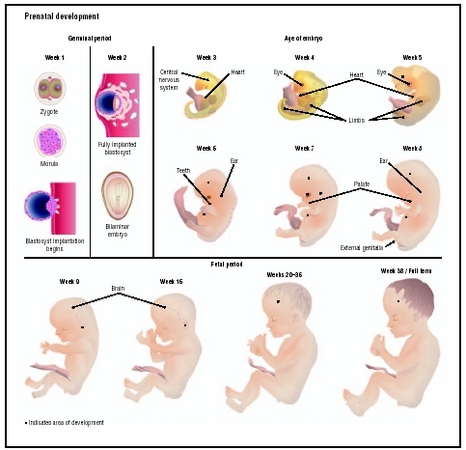
- Week 3: Beginning development of the brain, heart, blood cells, circulatory system, spinal cord, and digestive system.
- Week 4: Beginning development of bones, facial structures, and limbs (presence of arm and leg buds); continuing development of the heart (which begins to beat), brain, and nervous tissue.
- Week 5: Beginning development of eyes, nose, kidneys, lungs; continuing development of the heart (formation of valves), brain, nervous tissue, and digestive tract.
- Week 6: Beginning development of hands, feet, and digits; continuing development of brain, heart, and circulation system.
- Week 7: Beginning development of hair follicles, nipples, eyelids, and sex organs (testes or ovaries); first formation of urine in the kidneys and first evidence of brain waves.
- Week 8: Facial features more distinct, internal organs well developed, the brain can signal for muscles to move, heart development ends, external sex organs begin to form.
By the end of the embryonic stage, all essential external and internal structures have been formed. The embryo is now referred to as a fetus.
Fetal stage
Prenatal development is most dramatic during the fetal stage. When an embryo becomes a fetus at eight weeks, it is approximately 3 centimeters (1.2 inches) in length from crown to rump and weighs about 3 grams (0.1 ounce). By the time the fetus is considered full-term at 38 weeks gestation, he or she may be 50 centimeters (20 inches) or 3.3 kilograms (7.3 pounds). Although all of the organ systems were formed during embryonic development, they continue to develop and grow during the fetal stage. Examples of some of the major features of fetal development by week are as follows:
- Weeks 9–12: The fetus reaches approximately 8 cm. (3.2 in.) in length; the head is approximately half the size of the fetus. External features such as the face, neck, eyelids, limbs, digits, and genitals are well formed. The beginnings of teeth appear, and red blood cells begin to be produced in the liver. The fetus is able to make a fist.
- Weeks 13–15: The fetus reaches approximately 15 cm. (6 in.) in length. Fine hair called lanugo first develops on the head; structures such as the lungs, sweat glands, muscles, and bones continue to develop. The fetus is able to swallow and make sucking motions.
- Weeks 16–20: The fetus reaches approximately 20 cm. (8 in.) in length. Lanugo begins to cover all skin surfaces, and fat begins to develop under the skin. Features such as finger and toenails, eyebrows, and eyelashes appear. The fetus becomes more active, and the mother can sometimes begin to feel fetal movements at this stage.
- Weeks 21–24: The fetus reaches approximately 28.5 cm. (11.2 in.) in length and weighs approximately 0.7 kg (1 lb. 10 oz.). Hair grows longer on the head, and the eyebrows and eye lashes finish forming. The lungs continue to develop with the formation of air sac (alveoli); the eyes finish developing. A startle reflex develops at this time.
- Weeks 25–28: The fetus reaches approximately 38 cm. (15 in.) in length and weighs approximately 1.2 kg (2 lb. 11 oz.). The next few weeks mark a period of rapid brain and nervous system development. The fetus gains greater control over movements such as opening and closing eyelids and certain body functions. The lungs have developed sufficiently that air breathing is possible.
- Weeks 29–32: The fetus reaches approximately 38–43 cm. (15–17 in.) in length and weighs approximately 2 kg (4 lb. 6 oz.). Fat deposits become more pronounced under the skin. The lungs remain immature but breathing movements begin. The fetus's bones are developed but not yet hardened.
- Weeks 33–36: The fetus reaches approximately 41–48 cm. (16–19 in.) in length and weighs 2.6–3.0 kg (5 lb. 12 oz. to 6 lb. 12 oz.). Body fat continues to increase, lanugo begins to disappear, and fingernails are fully grown. The fetus has gained a high degree of control over body functions.
- Weeks 36–38: The fetus reaches 48–53 cm. (19–21 in.) in length is considered to be full-term by the end of this period. Lanugo has mostly disappeared and is replaced with thicker hair on the head. Fingernails have grown past the tips of the fingers. In a healthy fetus, all organ systems are functioning.
Common problems
Although 90 percent of babies born in the United States are considered healthy, abnormalities may arise during prenatal development that are considered congenital (inherited or due to a genetic abnormality) or environmental (such as material derived abnormalities). In other cases, problems may arise when a fetus is born prematurely.
Congenital abnormalities
In some cases abnormalities may arise during prenatal development that cause physical malformations or developmental delays or affect various parts of the body after the child is born. The cause may be a small mutation in or damage to the genetic material of cells, or a major chromosomal abnormality (each normal cell has two copies each of 23 strands [called chromosomes] of genetic material, and abnormalities can arise if there are three copies of a strand or only one). Sometimes the abnormality is inherited from one or both parents; in other cases, the defect occurs because of an error in prenatal development.
Some abnormalities are minor and do not affect the long-term prognosis once the child is born. At the other end of the spectrum, abnormalities may be so severe that fetal demise is inevitable. Approximately 10 to 15 percent of pregnancies end before the twentieth week, a process called miscarriage or spontaneous abortion; congenital abnormalities account for a significant proportion of miscarriages. Genetic abnormalities account for approximately 5 percent of miscarriages.
Maternal derived abnormalities
The age, health status, nutritional status, and environment of the mother are all closely tied to the health of a growing embryo or fetus. Some examples of environmental factors that may lead to developmental abnormalities include:
- Age: As of 2004, research showed that babies born to mothers between the ages of seventeen and thirty-five tend to be healthier. One reason is that the risk of certain congenital abnormalities such as Down syndrome increases with mother's age (particularly mothers over forty). Another reason is that the risk of having pregnancy or birth complications is greater with women over the age of thirty-five.
- Health status: In some cases a mother may pass a viral or bacterial infection to the fetus, such as in human immunodeficiency virus (HIV). In other cases, a mother's illness may cause congenital malformations; an example is rubella , which can cause heart defects, deafness, developmental delays, and other problems in a fetus if the mother contracts it during pregnancy.
- Nutritional status: A well-balanced diet rich in nutrients such as folic acid , calcium, iron, zinc, vitamin D, and the B vitamins is recommended for pregnant women. Certain vitamin and mineral deficiencies can interfere with normal prenatal development. For example, a deficiency in folic acid during the early stages of pregnancy may lead to neural tube defects such as spina bifida . Mothers are recommended to eat approximately 300 additional calories a day (above and beyond a normal non-pregnancy diet) to support the fetus's growth and development.
- Other environmental factors: Exposure to certain substances called teratogens (agents that may interfere with prenatal development) during pregnancy may cause embryonic or fetal malformations. Examples of teratogens include alcohol, thalidomide, cocaine, certain seizure medications, diethylstilbestrol (DES), and the anti-acne drug Accutane.
Prematurity
Advances in medical care have made it possible for many infants born prematurely to survive and develop normally. The earlier the gestational age, the greater the chance of death or significant medical problems. Whether or not a premature infant will survive is intimately tied to his or her gestational age:
- 21 weeks or less: 0 percent survival rate
- 22 weeks: 0–10 percent survival rate
- 23 weeks: 10–35 percent survival rate
- 24 weeks: 40–70 percent survival rate
- 25 weeks: 50–80 percent survival rate
- 26 weeks: 80–90 percent survival rate
- 27 weeks: greater than 90 percent survival rate
KEY TERMS
Miscarriage —Loss of the embryo or fetus and other products of pregnancy before the twentieth week. Often, early in a pregnancy, if the condition of the baby and/or the mother's uterus are not compatible with sustaining life, the pregnancy stops, and the contents of the uterus are expelled. For this reason, miscarriage is also referred to as spontaneous abortion.
Ovary —One of the two almond-shaped glands in the female reproductive system responsible for producing eggs and the sex hormones estrogen and progesterone.
Teratogen —Any drug, chemical, maternal disease, or exposure that can cause physical or functional defects in an exposed embryo or fetus.
Uterus —The female reproductive organ that contains and nourishes a fetus from implantation until birth. Also called the womb.
Parental concerns
Many parents have questions or concerns about the prenatal development of an existing or anticipated child and what steps they should take to ensure their child's health. During prenatal visits to an obstetrician, a pregnant mother should be educated in proper nutrition and prenatal care; often, prenatal vitamins are prescribed to avoid nutritional deficiencies. Prenatal testing is often recommended to parents-to-be as a means of assessing the fetus's health and the risk of developing certain conditions. Some common prenatal tests that relate to prenatal development are as follows:
- blood tests to check for diseases that could affect the fetus, such as HIV, hepatitis B , or other sexually transmitted diseases
- blood tests to check if the mother carries a protein called Rh factor on her red blood cells; if she does not and her baby does (determined by whether the father is Rh-positive or not), she will require treatment to prevent a potentially damaging reaction to the baby
- chorionic villus sampling, a prenatal test that takes a tiny sample of the placenta with a needle to test for chromosomal abnormalities
- nuchal fold or nuchal translucency screening test, which measures a small space at the back of the fetus's neck using ultrasound; fetuses with larger nuchal folds have a greater risk of having a chromosomal abnormality
- amniocentesis, a test that takes a sample of the fluid that surrounds the fetus in the uterus to identify certain genetic disorders, congenital malformations, or the maturity of the fetus's lungs
Resources
BOOKS
Gilbert, Scott F. Developmental Biology , 6th ed. Sunderland, MA: Sinauer Associates, Inc., 2000.
PERIODICALS
Miller, Sharon M., and Jeanne M. Isabel. "Prenatal Screening Tests Facilitate Risk Assessment." Medical Laboratory Observer 34, no. 2 (February 2002): 8–21.
ORGANIZATIONS
March of Dimes Birth Defects Foundation. 1275 Mamaroneck Ave., White Plains, NY 10605. Web site: http://www.marchofdimes.com.
National Institute of Child Health and Human Development (NICHD) Information Resource Center (IRC). PO Box 3006, Rockville, MD 20847. Web site: http://www.nichd.nih.gov.
WEB SITES
Hill, Mark. UNSW Embryology , 2004. Available online at http://embryology.med.unsw.edu.au (accessed December 11, 2004).
McPherson, Katrina. "Fetal Development." MedlinePlus , May 8, 2004. Available online at http://www.nlm.nih.gov/medlineplus/ency/article/002398.htm (accessed December 11, 2004).
Stephanie Dionne Sherk
Comment about this article, ask questions, or add new information about this topic: